Chapter 4 Human Coronaviruses and Pre-Existing Immunity
[This was my first controversial call that humans had pre-existing immunity due to exposure to other coronaviruses. Remember, this was 2020, before vaccines and before the CDC really lost our trust. This led to the de-platforming of my book. This is where things start to get good!]
Part of the reason we know so much about SARS-CoV-2 is that it belongs to a large family of coronaviruses that infect various animal species. Coronaviruses share a common evolutionary history; all diverged from a common ancestor at some point. However, just as whales and mice are both mammals but are very different, comparisons have their limits. Humans have six different coronaviruses of medical importance, and their effects vary widely from SARS-CoV-2. We can learn a lot about Covid-19 by studying other human coronaviruses and how they behave, but we must be cautious with these comparisons.
We’ll begin with the coronaviruses that have the potential to cause epidemics before moving on to the endemic ones responsible for the common cold. Finally, we’ll examine the possibility that humans may have some pre-existing immunity to SARS-CoV-2 due to cross-reactive immunity with non-Covid-19 coronaviruses. [Suggests natural immunity and perhaps why I was canceled on Amazon]
The virus SARS-CoV-1 causes Severe Acute Respiratory Syndrome (SARS). Scientists previously referred to the virus as SARS until 2019, when the naming convention was updated to include the virus responsible for Covid-19. As a result, we now have SARS caused by SARS-CoV-1 and Covid-19 caused by SARS-CoV-2. SARS triggered a pandemic scare in several countries from 2002 to 2004. With a high death rate, it killed about 8,000 people but has since been eradicated from human populations. SARS transferred from a horseshoe bat and was passed to humans through an intermediary, the palm civet—a nocturnal, weasel-like creature native to Asian rainforests.
There are many similarities between the diseases SARS and Covid-19. In fact, these two viruses are the most genetically similar of all human coronaviruses, and both originate from bat coronaviruses. But why did SARS burn itself out? Understanding this is important because COVID-19 is unlikely to have the same effect. [Even though we know in 2025 that Covid is lab-enhanced, bat DNA remains the source.]
Firstly, SARS makes people extremely ill. That is, folks usually end up in the ICU with viral pneumonia and sepsis. There is no asymptomatic or mild form of SARS. Second, SARS is only contagious once people are actually sick. Since you are not worried about asymptomatic or pre-symptomatic transmission, it’s much easier to do airborne isolation for people with SARS. In fact, we were so successful at preventing the transmission of SARS that it has been eliminated from the human population since 2004. Even though they are genetically very similar, SARS is not a good model for understanding Covid-19 because it is always severe and easy to contain through isolation.
There is a second human coronavirus that is not endemic to consider: Middle East Respiratory Syndrome (MERS). MERS is also known as Camel Flu and is caused by MERS-CoV, which is less closely related to SARS-CoV-1 and -2 than they are to each other. MERS also jumped species from bats but now resides in camels. When humans encounter camels infected with MERS-CoV, they can become dead-end hosts for the virus. That is, when humans contract MERS-CoV, we are incidental hosts and do not efficiently spread the virus. The virus spreads well from camel to camel but not from human to human.
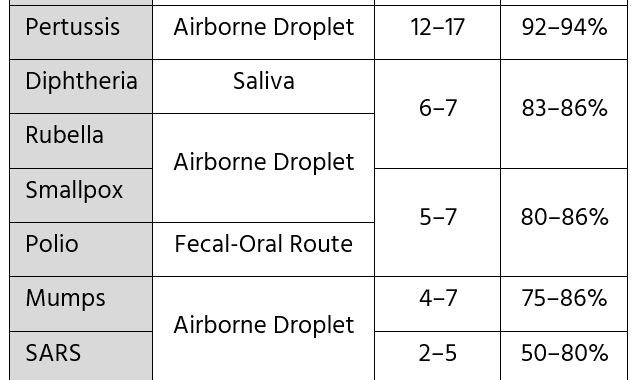
The main difference between MERS and Covid-19 is that human MERS isn’t very contagious, whereas Covid-19 spreads easily. MERS sometimes infects people through contact with camels, and when it does, it can cause severe illness with up to 35% mortality. Since it can survive well in camels, MERS won’t be eradicated until we vaccinate the camel hosts. It won’t start an outbreak in humans unless it becomes more efficient at spreading from person to person. MERS isn’t a good model for understanding Covid-19 because it is common in camels but rarely infects humans.
Endemic Human Coronaviruses
Endemic human coronaviruses operate a bit differently. Endemic, again, means they are always around. So, the endemic coronaviruses, also known as the common cold coronaviruses, are quite useful to study when trying to understand Covid-19. There are four strains of coronaviruses currently endemic in humans. They have friendly names, such as HCoV-NL63 and HCoV-OC43. The “HCoV” stands for human coronavirus, and the letters and numbers after the dash indicate the strain’s name. They circulate widely and year-round. In the past, we didn’t pay much attention to these four strains of endemic coronaviruses because of their harmless, omnipresent nature. If you swab enough noses in daycares at any time of year, you will find their genetic footprint. They cause infections with no symptoms, outbreaks of the common cold, and may also rarely lead to viral pneumonia, especially in those with underlying health conditions or immune issues. Rarely, endemic human coronaviruses kill opportunistically.
Coronavirus infections in children occur throughout the year, but outbreaks are most prevalent during the winter months. Some argue that coronaviruses are seasonal—more prevalent during winter, like influenza—but I believe that conclusion is based on incorrect evidence. Studies that only test for the virus when symptoms are present, unsurprisingly, find endemic coronaviruses more common during the respiratory infection season. After all, this is when people gather indoors and share air and viruses more often. However, studies that test year-round find endemic coronaviruses present all year.
In children, common cold coronaviruses are often co-pathogens. That is, during PCR testing, we detect a coronavirus along with another virus, such as RSV, influenza, rhinovirus, or various other detectable viruses. It is common to find an endemic coronavirus and another respiratory virus in children hospitalized with viral pneumonia. In adults, however, especially those with immunosuppression or lung disease, viral pneumonia caused by endemic coronaviruses is occasionally observed.
It appears that young children are generally protected from the severe consequences of endemic coronavirus. They may carry the virus in their noses, be infected without showing symptoms, or exhibit only mild symptoms, such as a runny nose. When considering hygiene in daycares, you might wonder why the infection doesn’t spread to all children. In other words, how is it possible that not all children have the virus all the time? For me, this still remains a bit of a mystery, a sort of immunological black box. There is an unexplained phenomenon about why young children don’t often get seriously ill from endemic coronaviruses. Children, relative to their exposure and immune development, seem to be largely spared. This is similar to what we observe in children with Covid-19, who also appear to be partly protected. This mystery is the focus of a future chapter.
Children develop some immunity to coronaviruses. After exposure, there is a relative immunity to each coronavirus strain, but this immunity diminishes over time. Additionally, there is cross-reactive protection between different strains. For example, having OC43 now can make you partially immune to NL63 for a while. So, how likely is it that there is some partial immunity to Covid-19 from endemic coronaviruses? It turns out that it is very likely, as we will discuss later. Generally, this is a common phenomenon with respiratory viruses.
It turns out that many examples of partial immunity come from previous infections with different viral strains. For instance, in the case of influenza, this is quite evident. During the 2009 H1N1 outbreak, elderly individuals were relatively protected from illness caused by this “novel” influenza strain because of their past exposure. These individuals had encountered the remnants of the 1918 influenza back in the 1960s, before that particular H1N1 strain was replaced by an H2 strain. Therefore, people who had influenza in 1960 were protected in 2009 when the H1N1 strain reappeared as a slightly altered version. This demonstrates the power of pre-existing immunity, where memory T-cells recall previous infections (or similar viruses) and quickly begin controlling the virus. We know that pre-existing immunity exists in endemic coronaviruses and see similar patterns in influenza. How can we apply this knowledge to better understand the effects of Covid-19?
Nature Reviews Immunology released a summary of recent immunological studies related to pre-existing immunity and Covid-19. Although I am not otherwise focusing on recent literature, this proof of concept is worth noting. This report finds that T-cells react due to SARS-CoV-2, and this was likely due to common cold coronaviruses. In fact, between 20% and 50% of people have cross-reactive T-cells present before any exposure to SARS-CoV-2. It was more common for the T-cells to recognize components shared by the viruses. This is big news! Somewhere between 20% and 50% of people have pre-existing immunity to Covid-19! In five different populations around the world, there is evidence that prior infection with endemic coronaviruses primes the immune system to respond to Covid-19.
Maybe this is why children do not often get sick from Covid-19. They are protected by frequent exposure to common cold coronaviruses. What is also unique about children and coronaviruses is that co-infection with other viruses is common among children who exhibit symptoms. This suggests that all coronaviruses may be less harmful in kids than in adults. Specifically, children may be more resilient to coronavirus infections than adults.
It is possible that common cold coronaviruses are not pathogens at all in children, but rather co-pathogens. If an endemic coronavirus happens to be present in your nose when you get a severe case of influenza, the test might detect both, even though only the influenza is actually causing the disease. Therefore, you could be infected with one virus while the true cause of the illness is a second pathogen. Certainly, we will learn more about the role of endemic coronaviruses in human disease over the next few years, but they will play a significant role in the Covid-19 pandemic.
Finally, we know these endemic coronaviruses are always present but tend to circulate in waves. There might be a common strain this year and a different one next year. These waves are thought to result from some cross-reactivity between strains, which provides partial, pre-existing immunity to other strains. The key point about immunity to coronaviruses is that it diminishes over time. You may have some partial protection from memory T-cells, but antibodies decrease. You can be infected again by the same strain of endemic coronavirus someday, but it probably won’t be as severe the second time.
It seems likely that asymptomatic children spread common cold coronaviruses. Covid-19 also has a unique quality, as you can be asymptomatic or presymptomatic and spread the virus 48 hours before you develop non-specific symptoms. That is, up to about 48 hours before showing any symptoms of an infection, you can be contagious. This is a major reason why Covid-19 is so infectious. You can spread it without knowing you have it or before any symptoms appear. In future chapters, we will see how this affects our ability to eradicate Covid-19, which gives us an idea of what the next few years might hold.
There is still a lot to learn, but it seems that a common cold coronavirus might protect you from getting Covid-19. Or, if you do catch it, perhaps you won’t be as sick. Even if there is cross-reactive immunity—which may modify the disease—it doesn’t last very long.